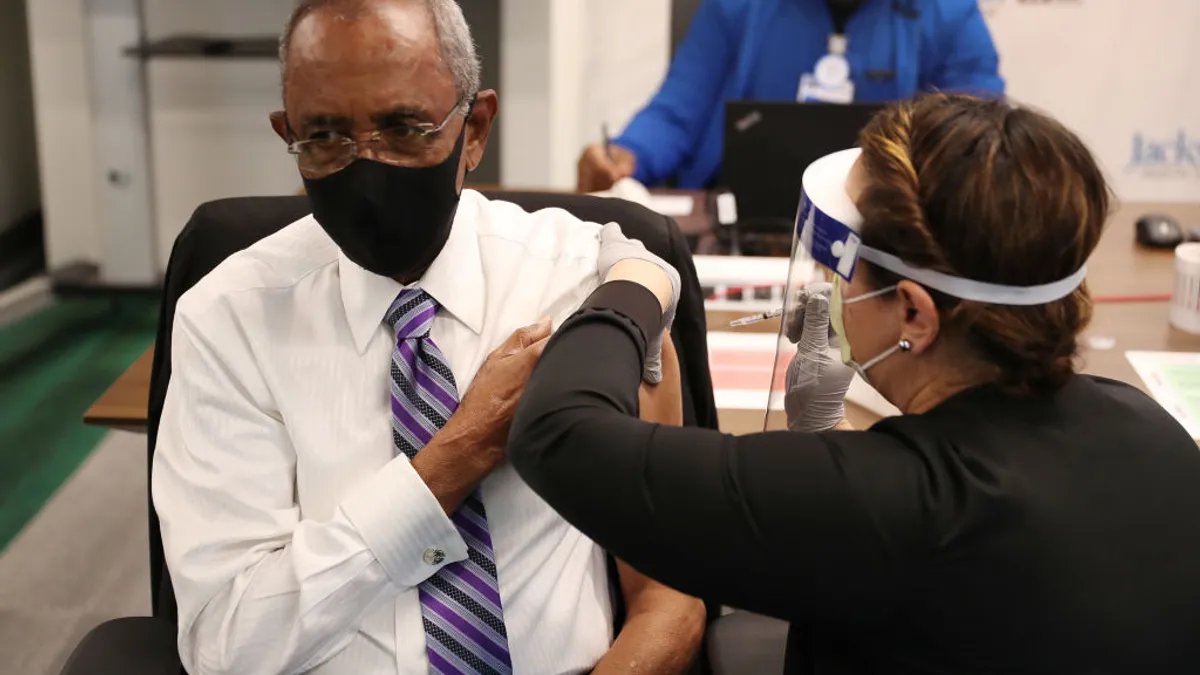
Frustrated by the emergence of the delta variant and a U.S. vaccination rate that has barely budged in the last few months, some employers are seeking alternatives.
First came incentives. Employers that sought to encourage vaccination offered employees paid time off, gift cards or other direct forms of payment, such as paying for transportation to and from a vaccination site. These incentives were particularly prevalent within industries dependent on in-person work, such as food service and retail.
Now, however, the focus has shifted toward a strategy commonly associated with smoking: health plan surcharges. Inquiries about increasing health insurance contribution costs for employees who choose not to get vaccinated are increasing, according to Wade Symons, partner at HR consulting firm Mercer and co-leader of its regulatory resource group. After first hearing murmurs from employers about vaccination surcharges, Symons said Mercer has been getting "at least one inquiry a day, sometimes more, about this concept."
The idea is not so much a consideration of last resort for employers as it is a potential way for those who have dangled incentives — or for those who have stayed "on the sidelines" as it pertains to COVID-19 vaccinations — to boost workplace health and safety, he added. It also may be an alternative to a vaccination mandate.
"My perspective is that employers are trying to do more to move that needle," Symons said, "and we've seen that what they've been doing gets you to a certain point, but vaccine levels are not where employers would have expected and wanted them to be, especially in some of those sectors where you have to have employees on the ground."
From an administrative perspective, vaccination surcharges are comparable to tobacco surcharges, Symons continued. Employees who smoke have the potential to drive higher costs to the employer's health plan, as do unvaccinated employees, or so the thinking goes.
Workplace safety is also a consideration. Whereas tobacco use mainly presents as a health problem for individual employees outside of the effects of secondhand smoke, vaccination can impact others in the workplace, Symons said.
Potential pitfalls
Sources who spoke to HR Dive are far from certain that a surcharge approach will be effective, however, and the strategy carries with it important practical and legal questions employers would need to address should they choose to adopt it.
For starters, employers will need to consider the timing of a surcharge given the coming open enrollment season. Those deadlines are complicated, Symons noted, because employers also are running up against deadlines to reopen physical worksites that are already threatened by the delta variant.
"This is something they want to do sooner than later," Symons said. "The question is, how long do you give someone to get vaccinated before the surcharge?"
There is also the issue of complying with limits on vaccination incentives and other wellness incentive regulations. In May, the U.S. Equal Employment Opportunity Commission published updated technical assistance stating that employers may offer incentives to employees to voluntarily receive a vaccine, whether an employee receives the vaccine on their own from a pharmacy, health department or community health partner, or whether the employee receives a vaccine administered by the employer or an agent of the employer.
But if the vaccine is administered by the employer or an agent of the employer, an incentive can only be offered under the Americans with Disabilities Act if it "is not so substantial as to be coercive," according to EEOC. The exact definition of what constitutes a coercive incentive is a "nebulous" term, Symons said, but he explained that employers should still be mindful of the restriction.
Surcharges, moreover, are also subject to the rules of the Affordable Care Act and HIPAA, which generally prohibit group health plans from charging similarly situated individuals different premiums or contributions, with the exception of certain wellness programs, according to the U.S. Department of Labor. Federal law divides wellness programs into one of two categories: participatory and health contingent. While it is unclear under which category a COVID-19 vaccination surcharge would fall, the most conservative standpoint would be to assume that it is a health-contingent wellness program, Symons said.
That implies a surcharge would need to follow federal requirements for health-contingent wellness programs. Under this example, the surcharge would need to be less than 30% of the cost of employee-only coverage under the health plan, but this can be a "pretty big number," Symons said. Most employers, he added, are considering a surcharge amount between $20 to $25 per paycheck, with those on the more extreme end considering up to $50 per paycheck.
Earlier this week, Delta Air Lines announced it would implement a $200 monthly health insurance surcharge for unvaccinated employees, The Wall Street Journal reported.
Employers also must offer a "reasonable alternative standard" to health-contingent wellness programs, and this requirement can differ depending on whether the program is considered an "activity-only" or "outcome-based" wellness program under federal law.
Though it is also unclear into which of these buckets vaccination surcharges would fall, Symons said a reasonable alternative may come in the form of allowing employees to watch a video on vaccine safety and the dangers of remaining unvaccinated, an alternative similar to that used for tobacco surcharges.
Others are not convinced that such alternatives would be effective, however. In an article published by Chief Executive, Willis Towers Watson officials Jeff Levin-Scherz and Julie Stone said that educational sessions "would not help improve the safety of the workplace," while even biweekly or weekly COVID-19 testing — which the authors called the "most clinically effective alternative" — would be difficult to implement due to the fact that employers may not know in advance of imposing the surcharge whether an employee has completed testing.
There are other potential issues beyond wellness program rules. For instance, a surcharge approach would not impact employees who waive health coverage by their employer, Levin-Scherz told HR Dive in an email. Additionally, such surcharges may be disproportionately imposed on low-wage workers, he noted, citing research showing that high vaccination rates are strongly correlated with education and income.
"Premium surcharges might make intuitive sense, but based on their structure they are unlikely to lead [to] a large increase in vaccination rates," Levin-Scherz said. "I believe employers will increasingly look at mandates, especially with the FDA formal full approval of the Pfizer vaccine."
Unanswered questions
Verification of an employee's vaccination status may create additional headaches. An Aug. 16 article published by the Society for Human Resource Management asked employers to consider how they would obtain proof of vaccination, given reports of false vaccination cards and a warning from the FBI regarding criminal activity with respect to making or buying such cards.
Verification is a tough question, Symons said; "I don't know how you deal with that." In the case of tobacco surcharge programs, he noted, employers tend to rely on an attestation from the employee that they have not used tobacco over a certain period of time. That approach may be easier than requiring physical proof, but it also may present administrative challenges, Symons said.
As with vaccination mandates, obtaining information about an employee's vaccination status for the purpose of a surcharge also necessitates caution, Symons said, due to the fact that this status is considered a confidential medical record.
Booster shots present another area of uncertainty. The Centers for Disease Control and Prevention recommended last week that people who are moderately to severely immunocompromised should receive an additional dose of an mRNA COVID-19 vaccine after the initial two doses, though the agency noted that this additional dose is not the same as a booster dose given to people when an immune response to a primary vaccine series is likely to have waned over time.
"I would presume that if we get a CDC recommendation that all should receive a booster shot, then I would think that would be added to the mandate or surcharge," Symons said. Assuming health insurance plans and employer plans would need to pay for a booster shot, employers may need to communicate that the shot will be paid for by the plan, he added.